
Scientists warn that it will take multiple methods to stop the disease, which is also known as breakbone fever and was once confined to the tropics.
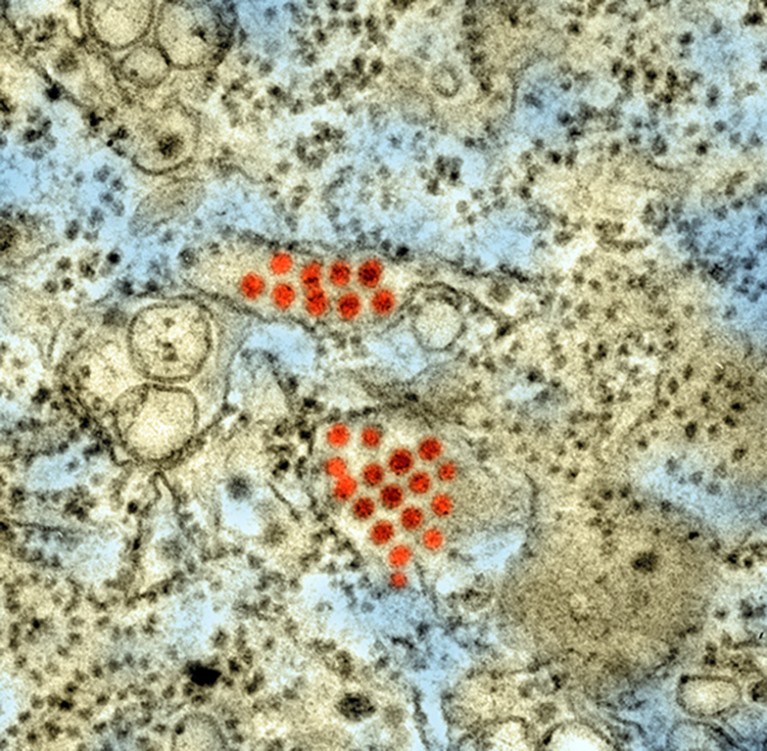
Particles of dengue virus (red; artificially coloured) infect a tissue specimen. Dengue mainly affects tropical regions but is spreading as temperatures warm.Credit: Science Source/SPL
Dengue is on the march. This year, more than 4.2 million cases of the disease, which is caused by a virus transmitted by mosquitoes, had been reported by 2 October, compared with half a million in 2000. And the disease, which was once confined to the tropics, is spreading to new locations around the world, including southern Europe.
There is no specific treatment for dengue, which is also known as breakbone fever and can cause fever, bone pain and even death. The available vaccines have important limitations, and controlling the mosquitoes that transmit the disease is challenging.
But scientists are not sitting idle. At the annual meeting of the American Society of Tropical Medicine and Hygiene, held in Chicago, Illinois, last month, researchers shared the latest results of their efforts to develop vaccines, antiviral medications and mosquito-control methods to curb the disease. Every available tool is needed, they say.
“We’re seeing the emergence of dengue in areas where we’ve never seen it before,” Adam Waickman, an immunologist at SUNY Upstate Medical University in Syracuse, New York, said during the meeting. “Effective dengue control is going to require multi-layered efforts.”
A key challenge for vaccine development is that dengue is caused by four distinct viral subtypes, or serotypes: DENV-1, DENV-2, DENV-3 and DENV-4. “The perfect dengue vaccine would have 90% efficacy across all different serotypes and would have the same level of efficacy for people who have had a previous dengue infection and those who have not,” says Timothy Endy, an immunologist also at SUNY Upstate Medical University. “We’re not there yet.”
Two dengue vaccines have received regulatory approvals so far. Dengvaxia, a vaccine made by Sanofi in Paris, has a 60% overall efficacy rate1 against symptomatic dengue, but it is only recommended for people who have had dengue before. This is because in those who have never been infected, the vaccine can actually exacerbate the risk of severe disease after infection through a mechanism called antibody-dependent enhancement.
Dengue is breaking records in the Americas — what’s behind the surge?
QDenga, a vaccine made by Takeda in Osaka, Japan, has so far been shown to be safe for people regardless of whether they have previously been infected, and it has an overall efficacy rate of 73% against symptomatic dengue2. But it has shown lower efficacy against DENV-3 and the results for DENV-4 remain inconclusive.
A third vaccine, TV003, has been developed by the US National Institute of Allergy and Infectious Diseases in Bethesda, Maryland. It is being tested by the Butantan Institute in São Paulo, Brazil, in a trial with more than 16,000 participants. According to data presented at the ASTMH meeting, for participants who had been followed for two to five years, TV003’s overall efficacy against symptomatic dengue was 80%.
“It also proved to be extremely safe, especially considering that almost half of the study population had never had dengue before,” says Maurício Nogueira, a microbiologist at the Faculty of Medicine of São José do Rio Preto in Brazil and an investigator working on the trial. But investigators lack data for some serotypes, because DENV-3 and DENV-4 did not circulate widely during the study period.
The vaccine could be useful for people who live in countries where the virus is endemic and also for people travelling to these areas, says Nogueira.
At the meeting, the pharmaceutical company Janssen in Beerse, Belgium, shared promising data on an antiviral drug called JNJ-1802 that is aimed at preventing dengue and is taken in pill form.
The data are from a ‘human challenge’ trial, in which volunteers are deliberately exposed to a pathogen in a controlled setting. Investigators gave healthy participants daily doses of either the antiviral drug or a placebo for 26 days. On the fifth day of treatment, participants were injected with dengue virus.
Scientist deliberately gave women Zika — here’s why
Six of the ten participants who received a high dose of the medication had no detectable virus in their blood throughout the study, whereas all of the placebo recipients had detectable levels of virus five days after receiving the dengue injection. Most participants who received low or medium doses of JNJ-1802 had detectable virus levels at some point, but a day or more later than the placebo group did.
The results support “further evaluation of JNJ-1802’s efficacy against natural infection with all dengue serotypes”, Anna Durbin, an infectious-disease specialist at the Johns Hopkins Bloomberg School of Public Health in Baltimore, Maryland, and a study investigator, said at the meeting.
But it might not be feasible to give a daily pill to whole populations in areas where the disease is endemic. This strategy might also be too expensive for many countries, says Endy. Moreover, most cases of dengue are asymptomatic, which means that many people would be taking medication to prevent a disease that would probably not give them any symptoms.
However, Durbin says that the drug could be useful to people travelling to areas where dengue is prevalent.
Standard measures to control dengue-transmitting mosquitoes, such as the use of insecticides, have had limited results. The dengue carrier Aedes aegypti “is an incredibly difficult mosquito to get rid of”, said Cameron Simmons, an infectious-disease specialist at the World Mosquito Program, a non-profit group in Melbourne, Australia, at the meeting. “The status quo is not good enough, so we need new interventions.” One such strategy is being trialled by the World Mosquito Program. The organization releases mosquitoes infected with Wolbachia, a bacterium that competes with viruses such as dengue and Zika, making the insects less likely to transmit these diseases. According to data presented at the meeting, city-wide deployment of modified mosquitoes in Colombia lowered the incidence of dengue by 94–97% in areas where the insects were well established.
doi: https://doi.org/10.1038/d41586-023-03453-0
